
Colon Cancer Treatment Doesn’t Have to Be Overwhelming
Imagine sitting in a doctor’s office, white walls, the faint smell of antiseptic in the air, and hearing the words: “You have colon cancer.” Yep, that moment hits like a freight train. Whether you’re the one with the diagnosis, a caregiver caught in the whirlwind, or just a health-conscious detective trying to stay ahead of the curve, it’s a lot. And if you’re anything like the rest of us, your brain probably skips ahead to one question: What’s the treatment?
Colon cancer treatment can feel like learning a new language overnight—one with a lot of big words, acronyms, and decisions you didn’t sign up to make. But here’s the thing: you don’t have to do it alone. This blog post is your crash course, your handbook, your coffee chat with a friend who happens to know a thing or two about this stuff.
We’re breaking down the treatment options for colon cancer—what they are, how they work, and how they change depending on the stage. We’ll sprinkle in some stats (not too scary, promise), walk through new advances, and make sure you walk away feeling informed and a little more in control.
Let’s face it: cancer isn’t exactly polite. But with the right info in your corner, you can absolutely stare it down.
Understanding Colon Cancer – A Quick Refresher
Okay, before we dive into the deep end of colon cancer treatment options, let’s get on the same page about what we’re dealing with here.
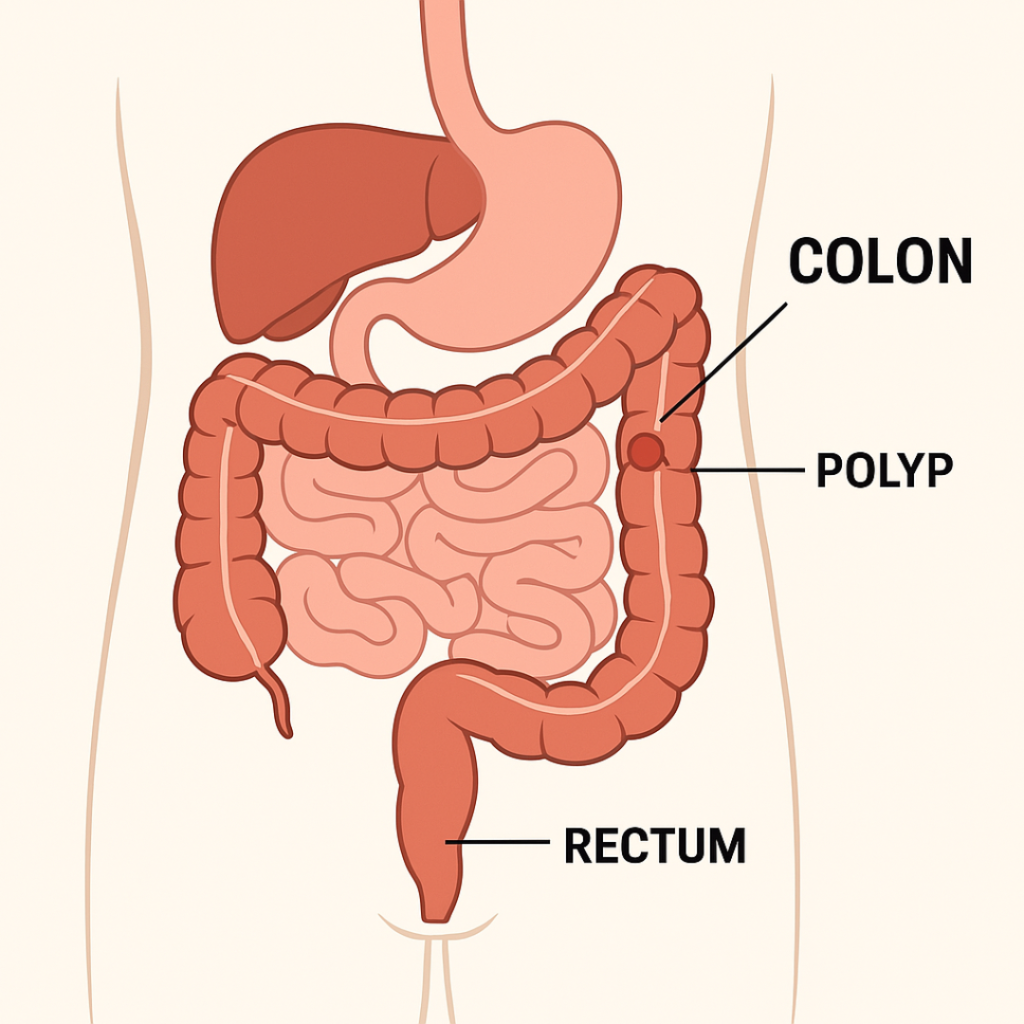
Colon cancer, also called colorectal cancer when it includes the rectum, starts in the large intestine—your body’s waste-management department. It processes what’s left after digestion and sends it packing. But sometimes, cells in the colon grow out of control, forming tumors. These can begin as harmless polyps but may develop into cancer over time, often without obvious symptoms. That’s why it’s so important to recognize the early signs of colon cancer before it progresses.
Here’s where things get interesting (and a bit science-y, but stick with me):
Not all colon cancers are the same. Your individual health and specific colon cancer risk factors—like age, diet, genetics, and inflammation—play a big role in determining your treatment plan.
Early detection is a game-changer. Following recommended colon cancer screening guidelines can catch it early—when the 5-year survival rate is about 91%, according to the American Cancer Society.
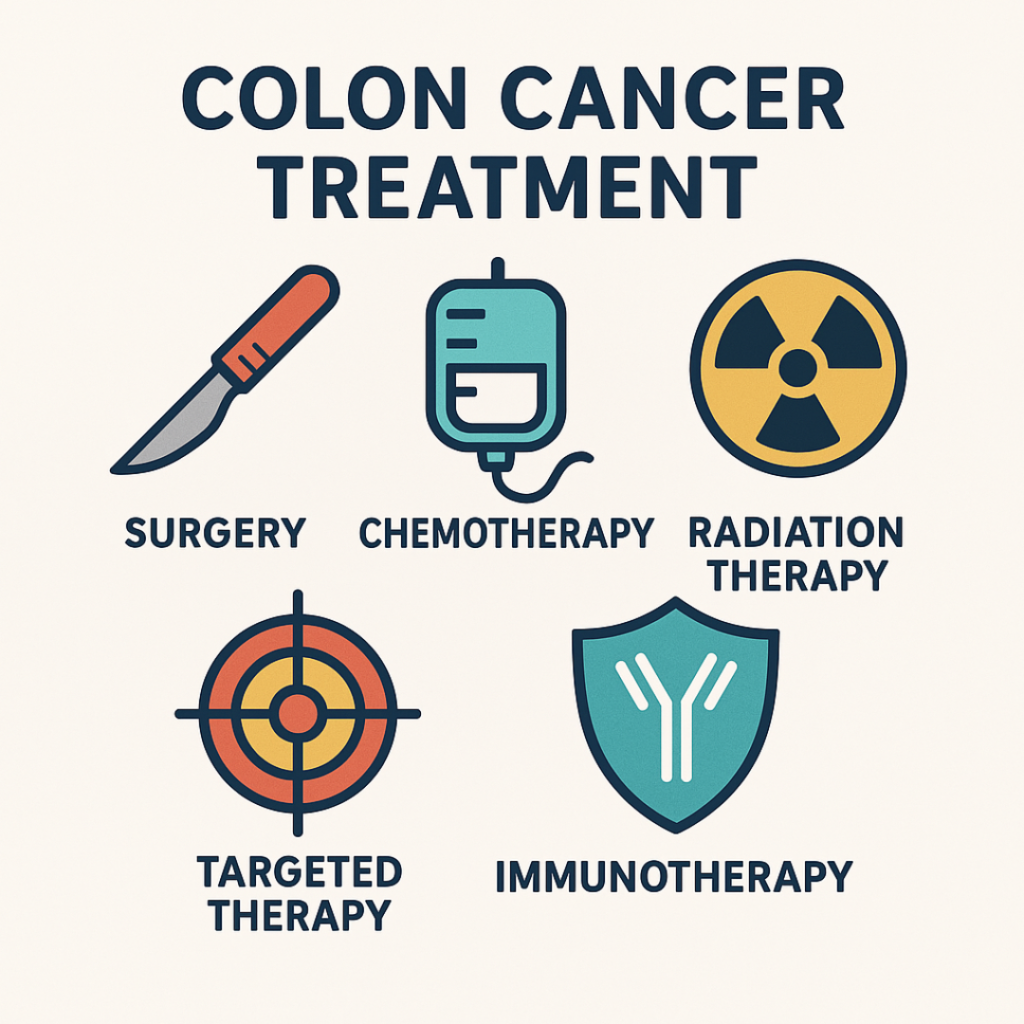
So when we say “colon cancer treatment,” we’re really talking about a whole toolkit—surgery, chemo, radiation, targeted therapy, even immunotherapy. And which tools get used depends on your unique situation.
Kind of like building IKEA furniture—you’ve got a manual, a bunch of parts, and the potential for a few “what the heck is this piece for?” moments. But we’ll guide you through it. Learn more about colon cancer symptoms
The Big Picture – Colon Cancer Treatment Options Explained
Alright, toolkit time. Let’s talk about the big players in the world of colon cancer treatment. Remember, most people don’t just get one type of treatment. It’s usually a combo—like cancer’s version of a tag team.
Here’s your lineup of colon cancer treatment options:
1. Surgery: The Main Event
If colon cancer were a party crasher, surgery is the bouncer. It’s often the first line of defense, especially if the cancer is localized (hasn’t spread).
Local excision or polypectomy: For early-stage cancer, doctors may remove the tumor during a colonoscopy.
Partial colectomy: Removes the cancerous part of the colon and reattaches the healthy ends. Most common.
Colostomy (sometimes): Creates an opening in the abdomen for waste to leave the body. Usually temporary, but sometimes permanent if reconnection isn’t possible.
Surgery is pretty effective, but it’s not always the end of the story—especially if cancer has wandered off to lymph nodes or beyond.
2. Chemotherapy: The System-Wide Sweep
Chemotherapy is the cleanup crew. It uses drugs to kill fast-growing cancer cells, and it’s often used:
After surgery to kill any leftover cells (called adjuvant therapy).
Before surgery to shrink large tumors (neoadjuvant therapy).
When cancer has spread, to slow growth and relieve symptoms.
Side effects? Yep. Nausea, fatigue, hair thinning—but they’re often manageable and temporary.
3. Radiation Therapy: Precision Zapping
Radiation therapy uses high-energy rays to target and destroy cancer cells. It’s more commonly used for rectal cancer than colon cancer, but it can be helpful:
To shrink tumors before surgery.
To reduce recurrence after surgery.
To ease pain or symptoms in later stages.
4. Targeted Therapy: Sniper Mode Activated
Instead of blasting all fast-growing cells like chemo does, targeted therapy zooms in on specific cancer cell features.
Examples: Bevacizumab (Avastin), cetuximab (Erbitux).
Works well for patients with specific gene mutations like KRAS or BRAF.
Think of it like GPS-guided missiles versus carpet bombing.
5. Immunotherapy: Training Your Body to Fight Back
This one’s the new kid on the block—and it’s exciting. Immunotherapy helps your immune system recognize and attack cancer.
Best for certain cases with microsatellite instability-high (MSI-H) or mismatch repair deficiency (dMMR) tumors.
Drugs like pembrolizumab (Keytruda) and nivolumab (Opdivo) are showing great promise.
Quick Recap:
Surgery = Remove the source.
Chemo = Clean up any stragglers.
Radiation = Pinpoint destruction.
Targeted therapy = Smart attacks.
Immunotherapy = Supercharge your body’s defenses.
It might sound like a Marvel movie plot—but this time, you’re the hero, and the treatment plan is your arsenal.
Staging & Strategy – How Colon Cancer Treatment Changes at Each Stage
Let’s break this down like a video game—with levels. The higher the stage, the tougher the fight.
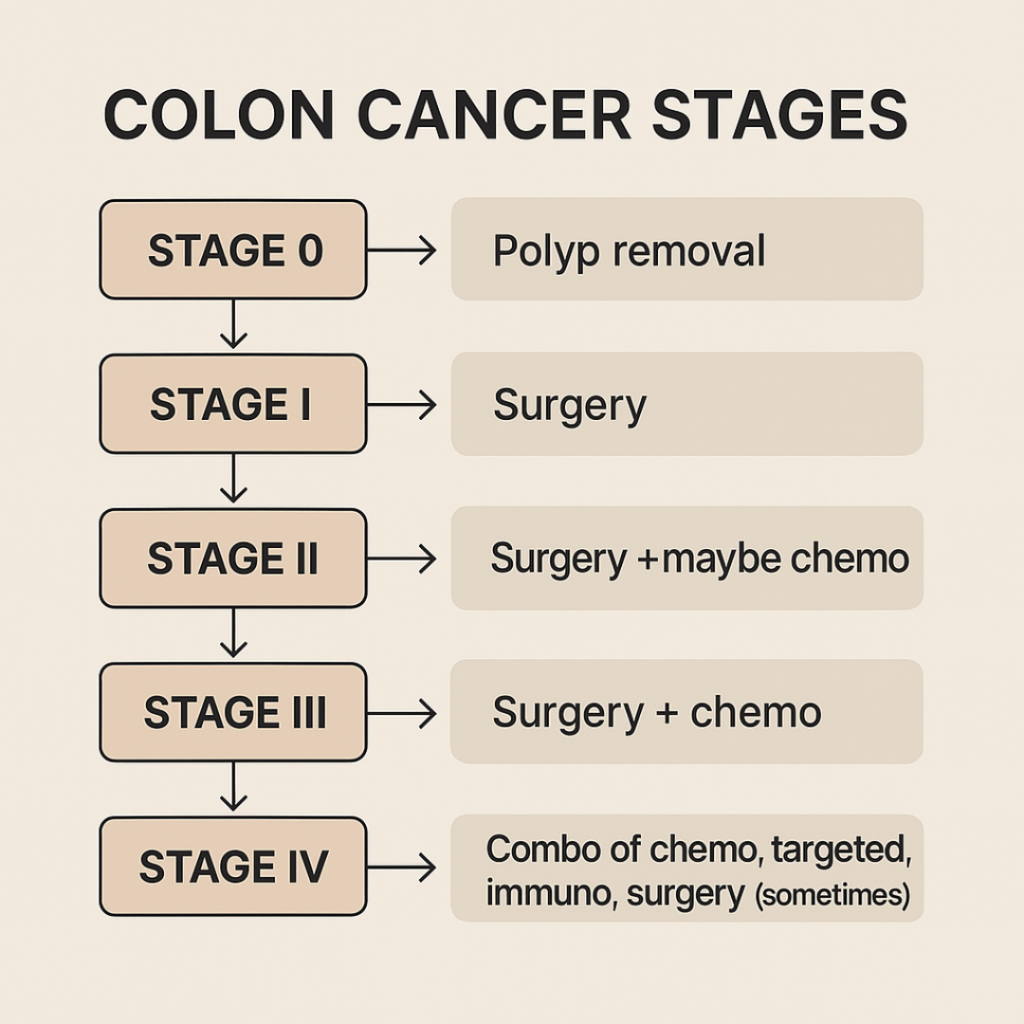
Here’s how colon cancer treatment shifts depending on where you are in the game:
Stage 0 (Carcinoma in situ):
Think of this as the cancer dipping its toe in the water. It hasn’t gone deep, and that’s great news.
Treatment: Usually just a polypectomy or local excision during a colonoscopy.
Outlook: Excellent. Most patients don’t need further treatment beyond regular screening.
Stage I:
The cancer has made itself at home in the colon wall but hasn’t invited the lymph nodes to the party.
Treatment: A colectomy to remove the cancerous section of the colon.
Chemo? Not usually needed unless there are high-risk features.
Stage II:
Now it’s getting serious. The tumor has grown deeper but still hasn’t hit the lymph nodes.
Treatment: Surgery is the main approach.
Chemotherapy: Sometimes used post-surgery, especially if:
The tumor looks aggressive.
There’s a chance it might come back.
You’re young and healthy enough to handle it.
Stage III:
Game-changer. The cancer has reached nearby lymph nodes, so we’re looking at a combo approach.
Treatment: Surgery to remove the tumor plus chemotherapy (usually FOLFOX or CAPOX regimens).
Radiation: Mostly used if the cancer involves the rectum or if there were close margins after surgery.
Stage IV (Metastatic):
Now we’re dealing with cancer that’s packed its bags and moved into other organs—commonly the liver or lungs.
Treatment: Highly customized.
Chemo is standard (to shrink tumors and slow growth).
Targeted therapy and immunotherapy may be added based on genetic testing.
Surgery might still be on the table—for example, if the liver has a limited number of tumors that can be removed.
Clinical trials: These can offer access to cutting-edge treatments.
Understanding your stage is key to forming a plan—and knowing where you stand in terms of colon cancer survival rates can help you prepare both emotionally and strategically.
TL;DR: Treatment by Stage
| Stage | Treatment Approach |
|---|---|
| 0 | Polyp removal |
| I | Surgery |
| II | Surgery + maybe chemo |
| III | Surgery + chemo |
| IV | Combo of chemo, targeted, immuno, surgery (sometimes) |
The goal? Match the intensity of the treatment with the reach of the disease. It’s not about throwing everything at it—it’s about being smart, strategic, and tailoring the approach to give the best shot at survival and quality of life.
Holistic Support – Beyond the Medical Side of Treatment
Let’s be real—colon cancer treatment isn’t just about surgery and medications. It’s about managing the whole you. Your mind, your energy, your gut (literally), and even your daily routine are all on this journey together.
So, what does “supportive care” actually mean? It’s the stuff that doesn’t always get the spotlight but can make a huge difference in how you feel during and after treatment. Let’s unpack it.
1. Nutrition: Feeding Your Body Through the Fight
When your colon’s the star of the show, food suddenly feels like a VIP. But chemo, surgery, or radiation can throw a wrench in digestion. Following some smart colon cancer prevention strategies can also support healing and help your gut stay strong during treatment.
Eat small, frequent meals to avoid bloating and nausea.
Lean proteins (think tofu, chicken, fish) help with healing.
Cooked veggies are easier on your system than raw ones.
Stay hydrated, especially during chemo.
Skip the greasy stuff—it’s not your colon’s BFF right now.
Pro tip: A registered dietitian who works with cancer patients is worth their weight in gold. They can create a plan that works with your treatment—not against it.
2. Mental Health: You’re Not Just a Patient, You’re a Person
Colon cancer therapy can feel like a full-time job. And just like any job, it comes with stress, burnout, and occasional “why me?” moments.
Therapy or support groups can help you vent, cry, laugh, and feel understood.
Mindfulness and meditation actually help reduce anxiety and pain perception.
Apps like Calm, Headspace, or even journaling can give your brain a breather.
Feeling down doesn’t make you weak—it makes you human.
3. Movement: Yes, Even a Little Helps
You don’t have to train for a marathon (unless you’re into that kind of thing). But light exercise—like walking, stretching, or yoga—can help with:
Reducing fatigue
Boosting mood
Improving digestion
Speeding up recovery
Start slow. Listen to your body. And if it says “nap,” take the nap.
4. Friends, Family, and Asking for Help
You know all those people who said, “Let me know if you need anything”? Time to cash in. Seriously.
Rides to appointments? Ask.
Meal prep? Yes, please.
Just someone to sit and binge old sitcoms with? Essential.
Let people show up for you. And don’t be shy about asking.
Colon cancer treatment isn’t just about killing cancer cells—it’s about keeping you strong enough to keep going. And that means treating your body like the resilient, amazing, slightly battle-worn warrior it is.
What’s New? Exciting Advances in Colon Cancer Treatment
If colon cancer treatment had a tech support line, you’d hear: “Please hold while we update your options.” Because honestly? The future of colon cancer therapy is looking pretty futuristic.
Over the past few years, science has been cooking up some impressive breakthroughs—giving doctors new tools, giving patients new hope, and giving cancer… well, a serious run for its money.
Here’s what’s new and exciting in the world of colon cancer treatment:
1. Immunotherapy Is Getting Smarter
We talked about immunotherapy earlier, but the way it’s evolving is mind-blowing.
Checkpoint inhibitors like pembrolizumab (Keytruda) are now approved for certain genetic profiles—specifically tumors that are MSI-H or dMMR. These types are more likely to respond well to immunotherapy.

Researchers are exploring combo therapies that boost immune response and reduce side effects.
📌 Why it matters: Traditional chemo attacks broadly. Immunotherapy tells your body to get specific—kind of like giving your immune system a “Most Wanted” poster.
2. Liquid Biopsies: Cancer Detection Without the Scalpels
A regular biopsy requires tissue. A liquid biopsy? Just a vial of blood. Doctors can now find tiny fragments of tumor DNA floating in your bloodstream.
It helps detect recurrence early.
It can help tailor ongoing treatment more precisely.
📌 Why it matters: More data, fewer invasive procedures. That’s a win.
3. Genetic & Molecular Testing
Want your treatment to be as customized as your Spotify playlist? Then genetic testing is your jam.
Doctors now analyze colon tumors for mutations like KRAS, NRAS, and BRAF.
Your mutation profile helps determine which targeted therapy you’re eligible for.
📌 Why it matters: Not every drug works for every person. These tests help doctors skip the trial-and-error and go straight to what works.
4. Artificial Intelligence (AI) in Cancer Treatment
AI isn’t just for writing your kid’s book report anymore. It’s helping doctors predict outcomes, recommend treatments, and even assist in surgery.
Some programs analyze pathology slides better than humans (no offense, humans).
Others recommend treatment regimens based on thousands of similar cases.
📌 Why it matters: Faster, smarter decisions—especially in complex or advanced cases.
5. Clinical Trials: Where the Magic Starts
No, you don’t have to be a guinea pig. Clinical trials are carefully designed, monitored, and often offer access to tomorrow’s treatment today.
You can search for colon cancer trials on sites like ClinicalTrials.gov or through your oncologist.
Some focus on stage IV cases. Others test add-on therapies for earlier stages.
📌 Why it matters: It’s a shot at cutting-edge care—and helps future patients, too.
Bottom line? Colon cancer treatment is no longer just about “cut it out and cross your fingers.” It’s about personalizing care, minimizing side effects, and staying five steps ahead of cancer’s next move.

Choosing the Right Path – How to Make Treatment Decisions
Colon cancer treatment isn’t a one-way street—it’s more like a choose-your-own-adventure book. Except, you know, with higher stakes. Every decision you make—from whether to go with surgery alone to adding chemotherapy, targeted drugs, or even clinical trials—shapes your story.
But how do you know what’s right for you?
Here’s how to navigate the crossroads without losing your mind (or your sense of humor):
1. Start with Questions (Lots of Them)
Your doctor isn’t just there to talk at you. They’re there to help you understand. Bring a notebook, a friend, or a phone to record the convo.
Good starter questions:
What stage is my cancer, and what does that mean?
What are my treatment options for colon cancer at this stage?
What are the risks and benefits of each treatment?
Are there clinical trials I qualify for?
What happens if I do nothing?
📌 Pro tip: Don’t be shy about asking “What would you do if you were me?” Sometimes doctors give the most honest advice when you flip the script.
2. Consider a Second Opinion
Even if you love your doctor more than your barista who knows your order by heart, it’s completely okay to get a second opinion. In fact, it’s smart.
It can confirm your treatment plan—or suggest another one.
Many major cancer centers (like MD Anderson, Mayo Clinic, and Sloan Kettering) offer virtual consults.
📌 Why it matters: Peace of mind is a powerful thing when your life is on the line.
3. Balance Treatment Goals with Quality of Life
Some people want to fight with every weapon available. Others prioritize comfort and quality time. Both are valid.
Ask yourself:
What does “success” look like for me?
How do I want to feel during treatment?
What am I willing—and not willing—to go through?
📌 Reminder: This is your life. You’re the captain here. Everyone else? Advisors.
4. Know Your Resources
Colon cancer treatment isn’t cheap. And navigating insurance, billing, and logistics is its own beast. You’re not alone, though:
Patient navigators can help you coordinate care.
Social workers can assist with travel, finances, and mental health.
Cancer-specific nonprofits (like Colorectal Cancer Alliance or CancerCare) offer everything from grants to support groups.
📌 Bookmark it: cancer.org and ccalliance.org have excellent guides.
5. Trust Your Gut (Even If It’s Healing)
You know you best. Yes, listen to the experts. But also listen to that inner voice—that sense of what feels right, what feels off, and what feels empowering.
Colon cancer treatment might be complex, but your role in it is simple: You’re the one driving the bus. Everyone else? Just here to help you find the best route.
Your Next Step – Empowerment Through Knowledge
If you’ve made it this far—first of all, gold star. Colon cancer treatment isn’t exactly light reading. But hopefully, now it feels a lot less like a tangled mess of medical jargon and a lot more like something you can understand, explore, and own.
Let’s rewind the highlight reel:
Colon cancer treatment is not one-size-fits-all. It depends on the stage, your overall health, and your unique genetic makeup.
Your main tools? Surgery, chemotherapy, radiation, targeted therapy, and immunotherapy—sometimes all working together like a medical Avengers team.
Treatment changes with each stage, from simple polyp removal at Stage 0 to combination therapies at Stage 4.
- There’s more to healing than medicine. Nutrition, mental health, movement, and community play a massive role.
- Exciting innovations—from AI-guided diagnostics to liquid biopsies—are turning what was once a scary unknown into a hopeful frontier.

You’re in charge of your care. Ask questions, get second opinions, weigh quality of life, and make the decision that’s right for you.
Caregivers are the unsung heroes. They need support just as much as the patient.
So… what now?
Here’s your next move:
👉 Bookmark this guide.
👉 Share it with someone who needs it.
👉 Explore other articles on our site to keep learning.
Knowledge won’t cure cancer—but it can help you make confident decisions, have stronger conversations with your doctor, and feel like you’re not just reacting… you’re responding with power. Want to learn how to spot cancer before it becomes serious? Head over to our Cancer Health Network and read Is Your Body Trying to Tell You Something? Recognizing the Early Signs of Cancer to explore the subtle symptoms your body might be using to wave a red flag.
Colon cancer is tough. But so are you. And now, you’ve got the information to back you up.
Let’s keep going—together.
